Pancreatic ductal adenocarcinoma (PDAC) is the third leading cause of cancer death in the United States and leads to well over 440,000 deaths per year Worldwide. Both the incidence and death rates of pancreatic cancer are increasing throughout the world. This year, an estimated 57,600 adults in the United States will be diagnosed with pancreatic cancer, 30,400 will be men and 27,350 women.
It is the fourth leading cause of cancer death in men and women. It accounts for 7% of all cancer deaths. As explained in the Introduction most pancreatic cancers (93%) are exocrine adenocarcinoma; 7% are pancreatic neuroendocrine tumors.
The 5-year survival rate describes what percent of people live at least 5 years after the cancer is found. The general 5-year survival rate for people with pancreatic cancer is 9%. Survival rates are based on many factors, including the specific stage of disease when it is diagnosed.
Pancreatic cancer is often difficult to diagnose. This is because there are no specific, cost-effective screening tests that can easily and reliably find early-stage pancreatic cancer in people who have no symptoms. This means it is often not found until later stages when the cancer can no longer be removed with surgery and has spread from the pancreas to other parts of the body.
If the cancer is detected at an early stage when surgical removal of the tumor is possible, the 5-year survival rate is 37%. About 10% of people are diagnosed at this stage. If the cancer has spread to surrounding tissues or organs, the 5-year survival rate is 12%. For the 53% of people who are diagnosed after the cancer has spread to a distant part of the body, the 5-year survival rate is 3%.
It is important to remember that statistics on the survival rates for people with pancreatic cancer are an estimate. The estimate comes from annual data based on the number of people with this cancer in the United States. Also, experts measure the survival statistics every 5 years. So the estimate may not show the results of better diagnosis or treatment available for less than 5 years.
Finally, in the U.S. alone more than 45,750 moms, dads, sisters, brothers, sons, and daughters will die this year of this horrific disease. These tragic facts have fueled the team at Vitalgenics to work harder than ever before for novel therapeutic approaches for this aggressive disease.
Statistics adapted from the American Cancer Society’s (ACS) publication, Cancer Facts & Figures 2020, and the ACS website (January 2020).
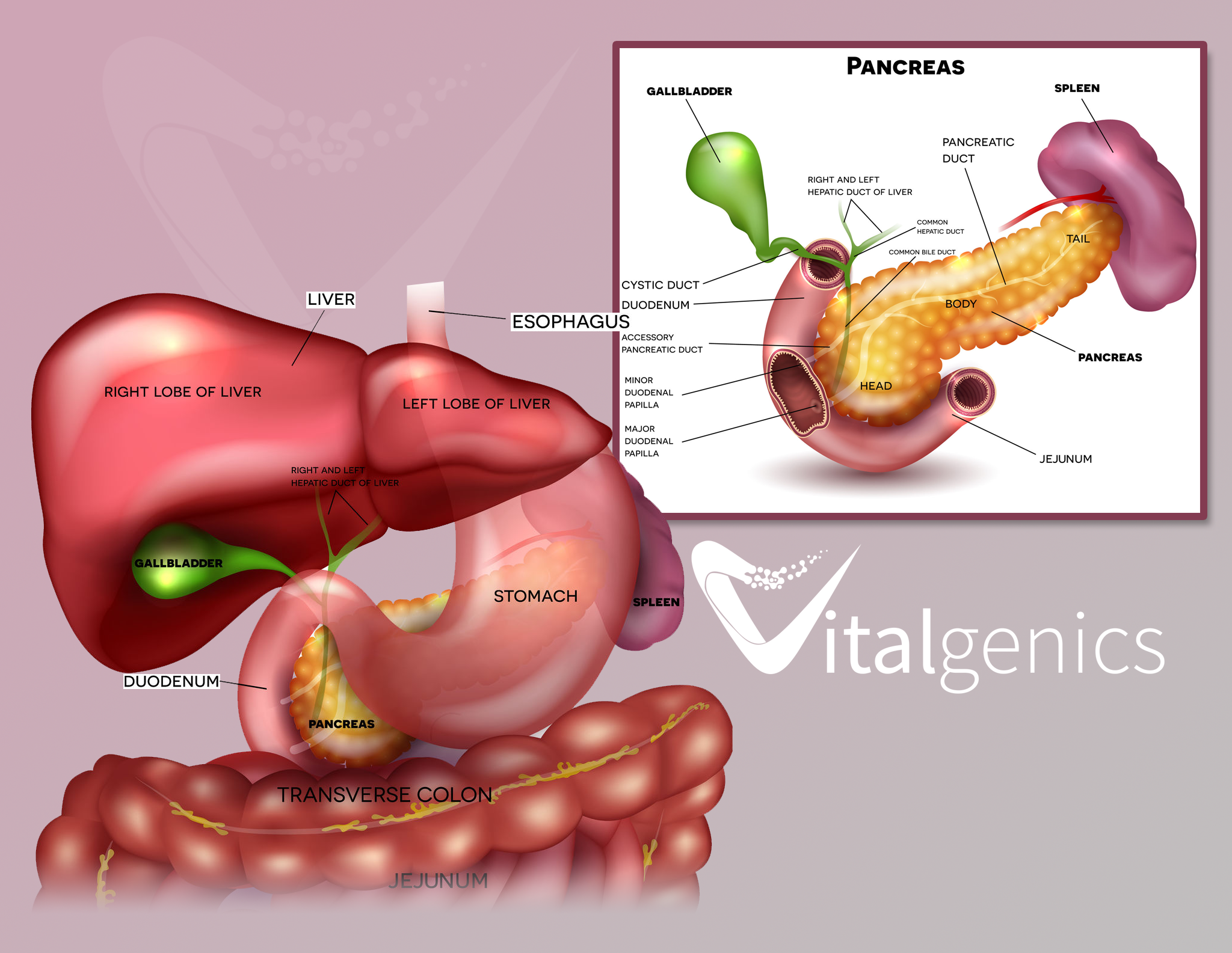
The pancreas is a gland located deep in the abdomen, between the stomach and the spine. It makes enzymes that help digestion and hormones that control blood-sugar levels.
Organs, like the pancreas, are made up of cells. Normally, cells divide to form new cells as the body needs them. When cells get old, they die, and new cells take their place. Sometimes this process breaks down. New cells form when the body does not need them, or old cells do not die. The extra cells may form a mass of tissue called a tumor.
Some tumors are benign. This means they are abnormal but cannot invade other parts of the body. A malignant tumor is called cancer. The cells grow out of control and can spread to other tissues and organs. Even when the cancer spreads to other areas of the body, it is still called pancreatic cancer if that is where it began. Pancreatic cancer often spreads to the liver, abdominal wall, lungs, bones and/or lymph nodes.
Doctors use staging as a way of describing where the cancer is located, where it has spread, and whether it is affecting other parts of the body. Diagnostic tests are used to find out the cancer’s stage. Determining the stage helps the doctor decide what type of treatment is best and can help predict a patient’s prognosis. There are different stage descriptions for different types of cancer. It is important for the staging to be done at a medical center with experience in staging pancreatic cancer. Doctors use several systems to stage pancreatic cancer with the most common being way to divide it into 4 categories based on whether it can be removed with surgery and where it has spread:
This type of pancreatic cancer can be surgically removed. Surgery is often done right after diagnosis. Sometimes, additional treatment may be recommended before surgery. The tumor may be located only in the pancreas or extend beyond it, but it has not grown into important arteries or veins in the area. There is no evidence that the tumor has spread to areas outside of the pancreas. Approximately 10% to 15% of patients are diagnosed with this stage.
This category describes a tumor that may be difficult or not possible to remove surgically when it is first diagnosed, but if chemotherapy and/or radiation therapy is able to shrink the tumor first, it may be able to be removed later with negative margins. A negative margin means that no visible cancer cells are left behind.
This type is still located only in the area around the pancreas, but it cannot be surgically removed because it has grown into or close to nearby arteries, veins, or nearby organs. This means that it cannot be removed with surgery because the risk of damaging these nearby structures is too high. There are no signs that it has spread to any distant parts of the body. Approximately 35% to 40% of patients are diagnosed with this stage.
The tumor has spread beyond the area of the pancreas and to other organs, such as the liver, lungs, or distant parts of the abdomen. Approximately 45% to 55% of patients are diagnosed with this stage.
By classifying each cancer into 1 of these categories, the health care team can plan the best treatment strategy.
Pancreatic tumors are either exocrine or neuroendocrine (endocrine) tumors. This is based on the type of cell they begin in. Understanding the type of tumor is very important because each type acts differently and responds to different treatments.
Approximately 93% of all pancreatic cancers are exocrine tumors with the most common type of pancreatic cancer being adenocarcinoma. About 7% of pancreatic tumors are neuroendocrine tumors (pancreatic NETs or PNETs), also called islet cell tumors.
Pancreatic Exocrine Tumors
About 93 percent of pancreatic cancers are exocrine tumors. They start in the exocrine cells of the pancreas, which produce enzymes that help with digestion.
Adenocarcinoma
As previously mentioned the most common type of pancreatic cancer is adenocarcinoma. Approximately 9 out of 10 people with pancreatic cancer have this type of cancer. Adenocarcinoma is an exocrine tumor. It starts in the cells lining the pancreatic duct, which make enzymes for digestion. Not to be confusing but the word “adenocarcinoma” alone can apply to cancer of other organs. If the cancer originated in the pancreas, it is always known as pancreatic adenocarcinoma.
Other Exocrine Tumors
Acinar cell carcinoma is a very rare form of pancreatic cancer.
Some tumors may cause the pancreas to make too much lipase, an enzyme that digests fats. Pancreatic lipase levels can be measured in the blood.
An intraductal papillary-mucinous neoplasm (IPMN) is a tumor that grows from the main pancreatic duct or from side branches of the duct. An IPMN may be benign (not cancer) when diagnosed. But, it has a chance of becoming cancer. This risk is high when the IPMN starts in the main pancreatic duct.
Mucinous cystic neoplasm with an invasive adenocarcinoma is a rare, cancerous tumor. It is a cyst filled with thick fluid. It is like an IPMN but is in just one part of the pancreas, usually the tail. These tumors are mostly in women. Mucinous cystic neoplasms can be benign (not cancer) if there is no invasive component. There are a few other rare exocrine tumor types.
Pancreatic Neuroendocrine Tumors (PNETs)
The balance or the remaining 7 percent of pancreatic tumors are neuroendocrine tumors (pancreatic NETs or PNETs), also called islet cell tumors. They often grow slower than exocrine tumors. PNETs come from the abnormal growth of endocrine cells in the pancreas called islet cells. These cells make hormones to control blood-sugar levels.
Pancreatic neuroendocrine tumors are either functional (produce hormones) or nonfunctional (do not produce hormones). Most PNETs are nonfunctional.
Pancreatic endocrine tumors have different symptoms, act differently and respond to different treatments than the more common pancreatic exocrine tumors.
PNETs are classified by the hormones they make. Common PNET types are:
- Gastrinoma (gastrin)
- Glucaganoma (glucagon)
- Insulinoma (insulin)
- Somatostatinoma (somatostatin)
- VIPoma (vasoactive intestinal peptide)
- Nonfunctional Islet Cell Tumor (no hormones)
Simply put changes in the homeostasis of the pancreas causes cancer. The changes that arise over time can happen because you were exposed to something harmful. They can also happen randomly. Up until now Pancreatic cancer’s exact causes were not well understood. Our etiology-centric approach has driven our ability to define the breakdown in the DNA and the cascading effect of the disease.
To give you an idea what the percentages look like about 5% to 10% of pancreatic cancers are considered familial or hereditary. Most pancreatic cancer happens randomly or is caused by things such as smoking, obesity and age.
Risk factors of developing pancreatic cancer are:
- Two or more first-degree relatives who have had pancreatic cancer
- A first-degree relative who developed pancreatic cancer before the age of 50
- An inherited genetic syndrome associated with pancreatic cancer
A person may also be more likely to get pancreatic cancer because of:
- Long-standing diabetes
- Chronic and hereditary pancreatitis
- Smoking
- Race (ethnicity): African-American or Ashkenazi Jew
- Age: over the age of 60
- Gender: males slightly more likely
- Diets high in red and processed meats
- Obesity
This does not mean that everyone who has these risk factors will get pancreatic cancer or that everyone who gets pancreatic cancer has one or more of these.
Signs and Symptoms of Pancreatic Cancer
Pancreatic cancer may cause only vague, unexplained symptoms, such as:
- Pain, usually in the abdomen or back
- Weight loss
- Jaundice (yellowing of the skin, eyes or both) with or without itching
- Loss of appetite
- Nausea
- Changes in stool
- Pancreatitis (swelling of the pancreas)
- Recent-onset diabetes
Fatigue, weakness and depression are also symptoms. A person with advanced pancreatic cancer may also have fluid in the abdomen and blood clots.
If symptoms are present, a doctor must do a few things to see if it is pancreatic cancer. The doctor will:
- Ask about the patient’s medical and family history
- Perform a physical exam, looking at patient’s body, skin and eyes and pressing on the abdomen to check for changes around the pancreas, liver and gallbladder
- Possibly order blood, urine and stool tests
- Order an imaging study, like a computed tomography (CT) scan or magnetic resonance imaging (MRI)
- Obtain tissue sample, called a biopsy
Pancreatic Imaging Tests
Imaging studies give doctors visual information about the pancreas and surrounding tissues. They are the only way to see a pancreatic tumor. So, imaging tests are critical in diagnosing and monitoring pancreatic cancer.
Doctors often use a computed tomography (CT) scan to see if the cancer has spread to nearby organs. A CT scan takes detailed pictures of the body.
Other imaging tests include:
- Magnetic Resonance Imaging (MRI): Uses radio waves and magnets to take pictures of organs and structures inside the body by measuring their energy
- Positron Emission Tomography (PET) Scan: Makes images based on the level of chemical reactions happening in cells
- Endoscopic Retrograde Cholangiopancreatography (ERCP): Takes x-ray pictures after a dye is injected through a thin tube
- Endoscopic Ultrasound (EUS): A thin tube, called an endoscope, with an ultrasound probe is passed through the patient’s mouth and into the stomach or duodenum to take pictures of the pancreas, bile duct and digestive tract
- Laparoscopy: A surgeon inserts a camera through a small cut in the abdomen to look at the organs
Blood Tests and Tumor Markers for Pancreatic Exocrine Tumors
Currently there is no blood test or tumor marker to find or diagnose pancreatic exocrine tumors, the most common type of pancreatic tumor.
A pancreatic tumor blocking the bile duct can cause higher bilirubin and liver enzyme levels in the blood. High levels of these substances in blood can be a clue for doctors to look for pancreatic cancer. But this does not happen in all pancreatic cancer patients.
After diagnosis, two blood tests may help your doctor see if your tumor is growing, staying the same or responding well to treatment. These tests measure substances some pancreatic cancer cells release into your blood, including:
- Carbohydrate antigen 19-9 (CA 19-9)
- Carcinoembryonic antigen (CEA)
Not all pancreatic tumors release these substances, and other cancer types and illnesses can also release them. So, they cannot be used to diagnose pancreatic cancer.
Blood Tests and Tumor Markers for Pancreatic Neuroendocrine Tumors
There is not one specific blood test that can find or diagnose pancreatic neuroendocrine tumors (PNETs). But some blood tests can help with diagnosis.
These tests measure:
- Chromogranin A (cgA): A molecule that is high in most people with PNETs
- Pancreatic polypeptide (PP): A hormone often high in people with PNETs
- Specific hormones made by pancreatic neuroendocrine tumors
Doctors can use these blood tests along with imaging tests to get more information to diagnose a pancreatic neuroendocrine tumor.
Biopsy
The only way for a doctor to know if a mass or tumor is cancer is to get a tissue sample, called a biopsy. A doctor can get a biopsy through surgery or procedures like endoscopic ultrasound (EUS) or endoscopic cholangiopancreatography (ERCP).
Then, a pathologist looks at the tissue samples under a microscope. The shape, size and arrangement of the cancer cells may help doctors determine the type of pancreatic cancer.
Molecular Profiling
After getting a tumor tissue sample, a doctor may run tests to understand the tumor’s biological details. This is called molecular profiling. The doctor may be able to use this information to make treatment decisions. Every pancreatic tumor is different. Patients who receive treatment based on their tumor’s biological characteristics have better outcomes.
Screening Tests
No universal screening tests for pancreatic cancer exist yet. But researchers across the country are studying people who have a high chance of getting pancreatic cancer.
It is recommended that a genetic counselor be contacted to determine the risk and eligibility for a screening program if a patient has:
- Two or more first-degree relatives who have had pancreatic cancer
- A first-degree relative who developed pancreatic cancer before the age of 50
- An inherited genetic syndrome associated with pancreatic cancer
The pancreas is located deep in the abdomen, so doctors usually cannot see or feel the tumor during a physical exam. Also, pancreatic cancer symptoms are not always obvious and usually develop over time. Doctors may use several tests to make a diagnosis. But, there is no standard test to diagnose pancreatic cancer. This makes diagnosis even more complicated.
Surgery currently offers the best chance of controlling pancreatic cancer for a long time. Because of the difficulty of diagnosing most patients are diagnosed at later stages and are not eligible for surgery. Tests to find pancreatic cancer in the earliest stages are urgently needed.
As our early detection study continues and as technology gets better, our researchers predict that we will make progress toward finding the disease earlier.
Another challenge is that pancreatic tumors are surrounded by a dense tissue layer, called the stroma. This makes it difficult for current treatment to reach the tumor. We are studying ways to get treatment through the stroma to make it more effective.
Also, some cancers have been successfully treated with targeted therapies which block specific mutations. But, until now these drugs have not been developed specifically for pancreatic cancer yet. Molecular Profiling tells you about the unique biology of your tumor. Results may align with targeted treatments that work well in other cancer types. As more studies are done, more targeted treatments will be developed and approved for pancreatic cancer patients whose tumors have specific molecular changes.
Pancreatic cancer may cause only vague unexplained symptoms. Pain (usually in the abdomen or back), weight loss, jaundice (yellowing of the skin and/or eyes) with or without itching, loss of appetite, nausea, change in stool, pancreatitis and recent-onset diabetes are symptoms that may indicate pancreatic cancer.
Pancreatic neuroendocrine tumors (PNETs) are rare, accounting for about 7 percent of all pancreatic tumors. PNETs may cause the pancreas to overproduce hormones. High levels of these hormones in the blood result in symptoms such as weight loss, nausea, vomiting, muscle weakness and skin rash.
Abdominal Bloating (Ascites)
Ascites is the abnormal accumulation of fluid in the abdomen. This extra fluid causes the belly to become swollen and distended.
Pain (Usually in the Abdomen or Back)
Pain in the upper abdomen or mid-back may be caused by the tumor pushing against or invading nerves or organs near the pancreas. Pain can also result if the tumor blocks the digestive tract.
Digestive Problems
Poor appetite, indigestion and nausea are common in people with pancreatic cancer. Some or all of these symptoms may occur when a tumor in the pancreas presses against the stomach or first portion of the small intestine. If this happens, food may remain in the stomach and cause several digestive difficulties, including nausea and vomiting. Digestive symptoms can also occur due to blockage of the pancreatic duct through which the pancreatic enzymes flow or due to changes in pancreatic enzyme production.
Jaundice
Jaundice is a yellowing of the skin and eyes caused by excess bilirubin (a component of bile) in the blood. A tumor in the head of the pancreas can cause narrowing of the bile duct and block the bile flowing from the gallbladder into the small intestine. Blockage of the bile duct causes a buildup of bilirubin. People with jaundice may also experience itchiness of the skin, abnormally dark urine and light or clay-colored stools.
Changes in Stools
Many pancreatic cancer patients experience diarrhea, constipation or both. Diarrhea consisting of loose, watery, oily or foul-smelling stools can be caused by insufficient amounts of pancreatic enzymes in the intestines. This leads to malabsorption as undigested food passes quickly through the digestive tract. Constipation is also a common problem, particularly in patients taking pain medications. These medications slow the passage of food through the intestines. If the digestive system works too slowly, it can cause stools to become dry, hard and difficult to pass.
Unexplained Weight Loss
Cancer-induced weight loss (also known as cancer cachexia) is a complex problem that affects the way the body uses calories and protein. Cancer cachexia can cause the body to burn more calories than usual, break down muscle and decrease appetite. A person may also notice a change in appetite or desire for certain foods.
Blood Clots
Cancer causes changes in the blood that can increase the likelihood of forming clots. Blood clots may go unnoticed and cause no symptoms. However, they are often associated with swelling, pain and tenderness in the affected area.
Diabetes
Diabetes is a condition in which the body does not make, or properly use, a pancreatic hormone called insulin. Insulin helps the body use glucose (sugar) efficiently. Research suggests that a sudden onset of type 2 diabetes in people age 50 or older may be an early symptom of pancreatic cancer, especially in those who have a low body mass index (BMI), experience continuous weight loss or do not have a family history of diabetes. A sudden change in blood sugar levels in diabetics who previously had well-controlled diabetes may also be a sign of pancreatic cancer.